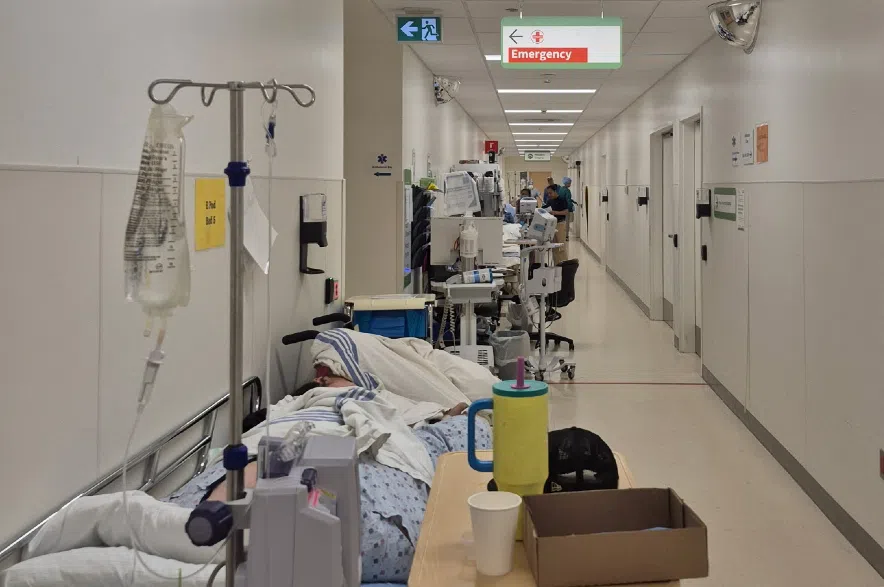
When video footage from Saskatoon’s Royal University Hospital first appeared online in late September, it stunned people across the province.
The short clip, filmed Sept. 25 and published below, showed stretchers pressed against walls, nurses dodging rolling beds, and patients packed so tightly into corridors that there was barely room to pass.
Within days, it had been viewed more than 100,000 times, drawing outrage and disbelief.
Read more:
- Regina medical clinic closing down for lack of doctors
- Saskatchewan NDP looks for ‘big, bold’ solution to health-care problems
- Sask. NDP to introduce legislation on ER closure notices
The Saskatchewan Health Authority quickly issued a statement saying the images reflected “an unprecedented level of demand” on emergency rooms. But for one Unity family, the pictures were déjà vu.
(Video and captions by Lynn Harmon. 650 CKOM blurred the faces of the people in the video to protect their identity.)
Weeks after the clip spread online, the NDP facilitated a one-on-one conversation between CJME and Tim Lang, whose 82-year-old mother had spent three days in a Royal University Hospital hallway under the same conditions.
Lang still remembers the day everything started.
“Monday, Sept. 22, around noon, my mother had a stroke,” he said. “We called the ambulance. They picked her up and took her straight to North Battleford Union Hospital for a CT scan.”
Doctors there reviewed the images and contacted the neurology department in Saskatoon.
“They said, ‘Bring her in right away by ambulance,’ because they couldn’t tell the damage on the CT,” Lang said.
Lang’s mother had survived a stroke six years earlier, so doctors needed an MRI to separate new damage from old.
By that evening, the family was following an ambulance east on Highway 16.
‘People lined up in hallways’
When they arrived at RUH, Lang said the reality of the province’s busiest emergency department became clear almost immediately.
“They parked her in the hallway right in front of the nurse’s station,” Lang said. “You wouldn’t believe it, people (were) lined up in the hallways like you wouldn’t believe.”
Every room was packed. Curtains divided patients where walls should have been. Stretchers were tucked into any space that could hold them.
Lang said nurses were doing their best, checking vitals and trying to comfort patients. Still, the sheer number of people made even small things feel impossible.
“They told her to use a bedpan, which she refused,” Lang said. “She said, ‘I’m not using a bedpan, get me up so I can sit on a toilet.’ They brought a commode in for her, let her do her business, and that was fine.”
But that moment of dignity didn’t last.
“She needed the washroom again later, and the nurse basically said, ‘You’re not strong enough to get up, you have to use a bedpan,’ which she refused again,” Lang said.
“They said, ‘No, you can’t get out of bed, we’ll have to put a catheter in you.’ She totally refused and fought tooth and nail. After about two hours of fighting, they finally gave her some Ativan (medication) to settle her down so they could put a catheter in.”
Lang and his wife stayed with his mother late into the night.
“We left around 1:30 a.m. because she’d finally settled down,” he said. “I gave the nurse my number and told them to call if she woke up.”
Patients just never stopped coming
When he came back at dawn, his mother was still in the hallway.
“She was awake and with it that morning, remembered things, doing fairly well,” he said.
“We spent most of the day with her watching what I’d call the gong show in the emergency room.”
He said there seemed to be more security staff than janitors, and the number of patients coming through the doors never stopped.
“The security in that RUH was just amazing trying to keep the riff-raff out of the hospital there.”
That night, Lang tucked his mother in around 10 p.m.
“She was fine that night, settled down,” he said. He left his phone number again and returned to the hotel.
When he came back at 6 a.m. the next morning, her bed was gone.
“I thought right away, ‘Oh, she must have got a room,’ ” he said. “I went to the nurse’s station and asked where she was. The nurse said, ‘Who are you talking about?’ and handed me a phone number to call.”
As he began to protest, another staff member overheard him. “He said, ‘You’re looking for Mrs. Lang? Follow me.”
Lang followed the staff member through a set of double doors and into another corridor, the main artery connecting the emergency department to the rest of the hospital.
“That hallway is lined with beds, wall to wall,” he said. “People come in and out, food carts, oxygen tanks, stretchers. It’s just a constant flow.”
There, between the flow of traffic, he found his mother’s bed.
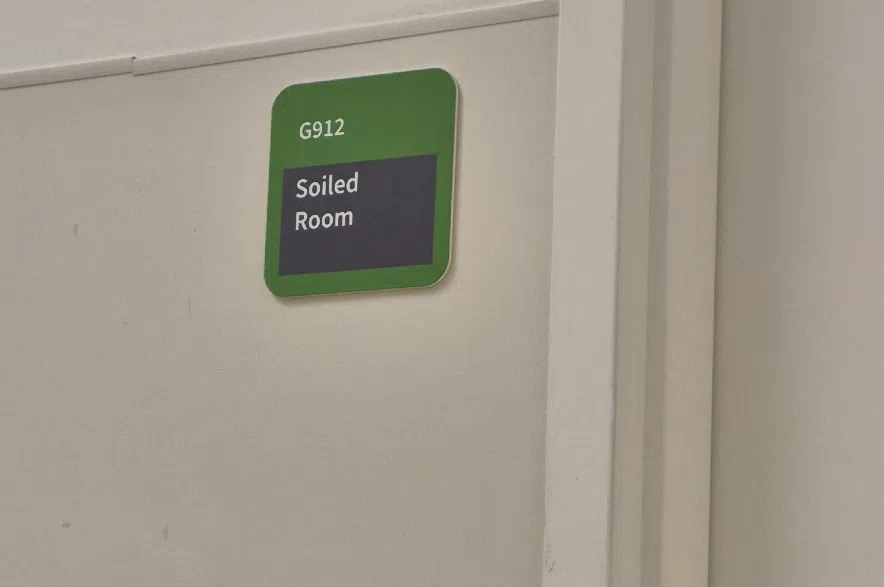
Tim Lang’s mothers bed was parked outside a room labelled “soiled room,” which he said smelled bad. (Tim Lang/Submitted)
Chaos spills over to hallways
“She hadn’t slept all night,” Lang said. “She told me she asked for water three or four times and never got any. She said, ‘There’s so many people around here. It stinks, it really smells.”
Across from her was a door marked Soiled Room.
“The smell coming out of there was bad,” he said. “The floor was dirty. Sheets were thrown down. It wasn’t clean at all.”
He noticed a therapy dog with a handler making rounds.
“The dog peed on the floor,” Lang said. “They threw a sheet over it and everyone walked over it for about two hours before somebody finally picked it up.”
That was one of the only times he saw anyone attempt to clean.
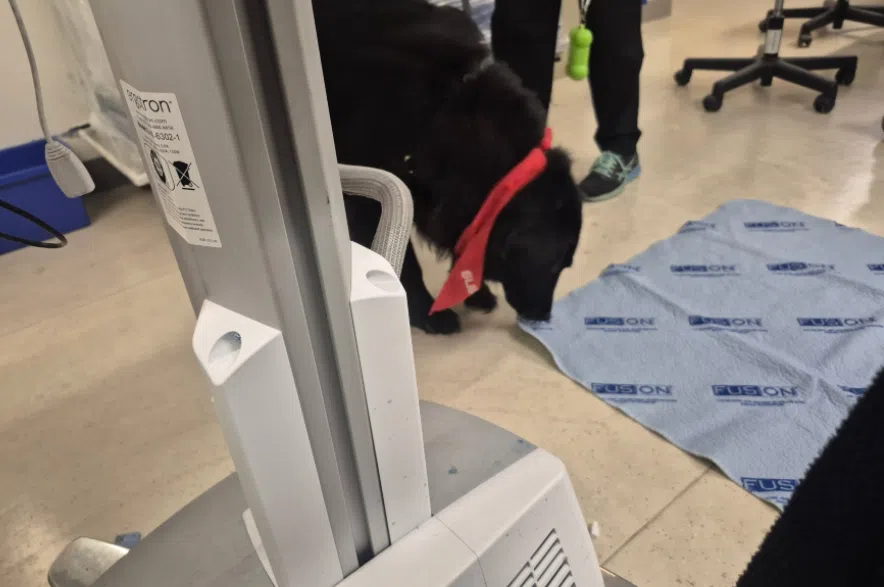
Tim Lang said a therapy dog peed on the floor in the corridor and was left for two hours. (Tim Lang/Submitted)
“In three days, I saw one dry mop go down that hallway,” he said. “Didn’t mop around the beds or anything, just the main walkway.”
Lang said the noise of the ER never stopped, with IV stands rattling, monitors beeping, stretchers bumping the walls.
“Between 11 p.m. and 12 a.m. I counted 55 people went by her bed,” he said. “The next morning, between 7 a.m. and 8 a.m., 172 people went by. Food trays, oxygen tanks, patients going for scans, just constant.”
Lang said the bedside table, which held her food and water, was touched “probably 100 times a day” by people squeezing past.
“In three days that table never did get wiped,” he said.
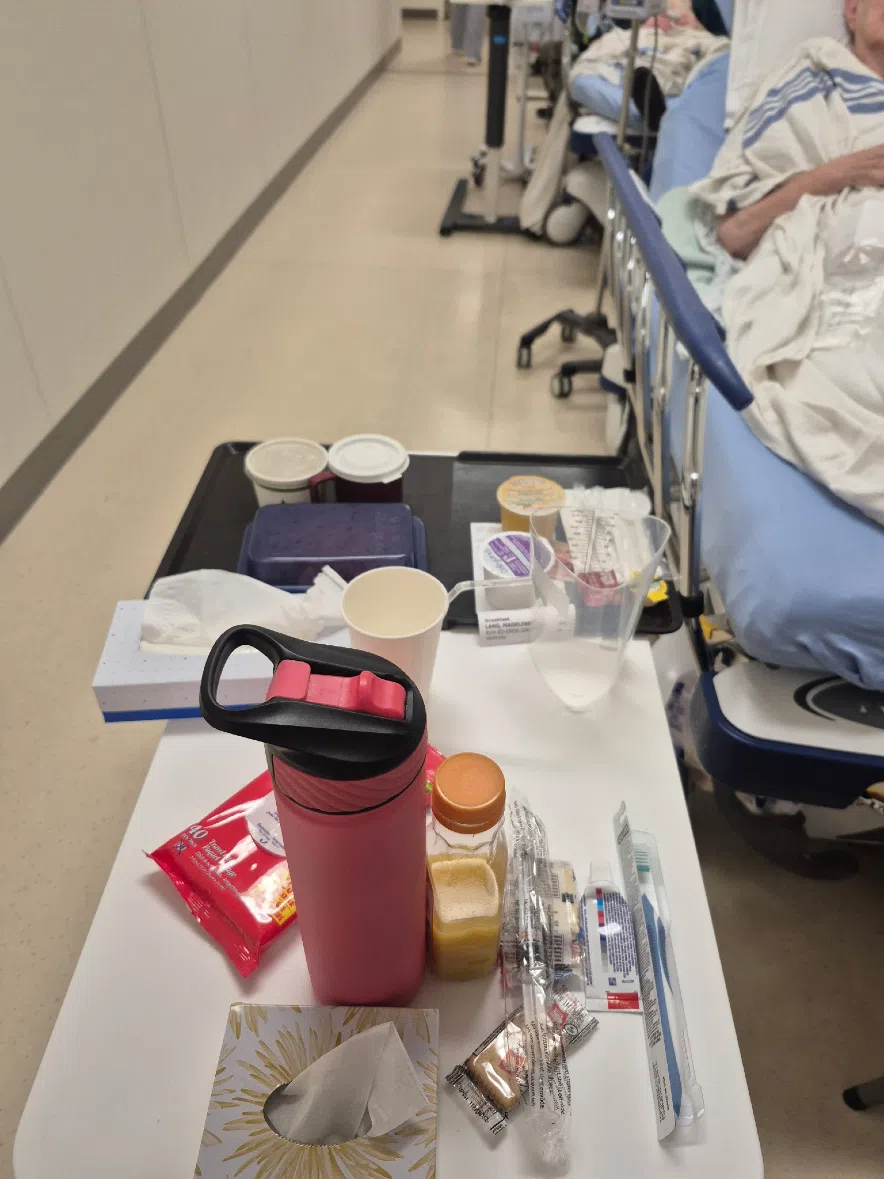
Tim Lang said his mother’s bedside table, which held her food and water, was touched “probably 100 times a day” by people squeezing past. (Tim Lang/Submitted)
Sleep, he said, was impossible for his mother.
“She was up all night, every night. They kept saying they’d get her a drink of water and never did. She was exhausted.”
Lang said after nearly three days in the hallway, a neurologist ordered an MRI, but it almost didn’t happen.
“They almost cancelled it because somebody forgot the order,” he said.
“Her neurologist happened to walk by. I hollered her back and told her they were going to cancel it. She said, ‘no way.’ She got the Ativan ordered and they did it.”
That night, his mother was moved upstairs to a room on the sixth floor.
“She finally got some sleep, had a meal, and you could see her settle down,” Lang said.
“She said, ‘I think I’m in heaven.’ She done a 180-spin in a matter of eight hours.”
Lang said it was the first time in days his mother had been able to stand up and walk to the bathroom.
“They got her up, got her cleaned, and she just looked like a different person,” he said. “She looked alive again.”
Signs of strain at RUH
Even then, the family saw signs of how strained the hospital had become.
“There’s two banks of two elevators in that hospital,” Lang said. “Two of them were out of order, and the other two were loaded down with everybody, staff, patients, visitors, stretchers.”
He said one nurse told him an elevator had been broken for years.
“She said one’s been out a couple of years, the other a couple of weeks,” Lang said. “Just no care in there at all.”
Through it all, Lang said he never blamed the front-line staff. He wants more support for those with mental health and addiction issues.
“In the ER department, in my opinion, they are overloaded with mental health issues and substance abuse,” Lang said.
“They’re working flat out, but the system’s overloaded … there’s just no room left.”
Lang said he saw the toll it took on both patients and workers.
“You have to go and experience it yourself,” he said.
Lang’s mother was eventually transferred back to Unity, where she’s been recovering.
“You never think it’s going to happen to you, that your mom’s going to be lying in a hallway like that,” he said. “It’s something I’ll never forget.”
SHA blames staff shortages, early flu season
The Saskatchewan Health Authority said the viral video and stories like Lang’s reflect the pressures staff are facing across the province.
In a statement, the SHA said hospitals are “implementing operational measures to manage patient flow and ensure care continues safely.”
John Ash, the SHA’s vice-president for integrated Saskatoon health, said at one point RUH had 42 patients waiting for inpatient beds. He cited staff shortages, an early flu season and ongoing capacity challenges.
Ash said the province’s March announcement of 109 new acute-care beds for Saskatoon City Hospital, with 20 already open, was part of the plan to help reduce pressure on emergency departments.
“We know these pressures are felt by both patients and staff,” the SHA said. “Our teams are doing everything they can to provide safe, timely care.”
Lang said he believes that.
“They’re trying,” he said. “They just don’t have enough. Nobody should have to go through that.”
Read more: